U.S. prepared for Ebola—10 patients at a time

Have you wondered why Ebola patients are being sent to Omaha, Nebraska? It’s because one physician, Dr. Philip Smith, had the foresight to set up the Nebraska Biocontainment Patient Care Unit after the 9/11 attacks as a bulwark against bioterrorism. Empty for more than a decade, used only for drills, it was called “Maurer’s Folly,” for Harold Maurer, former chancellor of the University of Nebraska Medical Center. The unit has a special air handling system to keep germs from escaping from patient rooms, and a steam sterilizer for scrubs and equipment. It could handle at most 10 patients at a time, but one or two would be more comfortable, owing to the large volume of infectious waste. It is the largest of only four such units in the U.S., and the only one designated for the general public.

Some say this is “overkill”—that our medical workers can be kept safe with much less stringent precautions. Ebola is “hard to get.” It is being compared to AIDS, which has not proved to be a significant threat to medical workers, not even surgeons. “The Ebola outbreak is presenting some of the same challenges we saw with HIV,” writes Cheryl Clark for HealthLeaders Media, such as “fear of contagion.” “In many ways, the AIDS epidemic in the early 1980s was the best thing to happen to healthcare,” she claims. For one thing, it brought “universal precautions.” CDC Director Dr. Tom Frieden also likens Ebola to AIDS. "In the 30 years I've been working in public health, the only thing like this has been AIDS," he said at a World Bank and International Monetary Fund annual meeting in Washington, D.C. “And we have to work now so that this is not the world's next AIDS.” Ebola, however, has far greater disaster potential than AIDS. Here are six major differences:
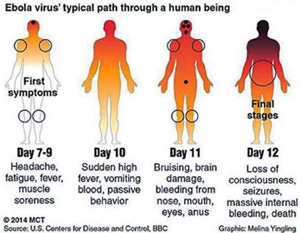
• Universal precautions are mostly adequate for AIDS, which really does seem to be “hard to get.” But despite protective gear, hundreds of nurses and doctors have become infected with Ebola and died in Africa—and so far one is infected in Spain. • AIDS, at least in the U.S., can be almost completely avoided by refraining from certain behaviors: needle sharing, and intimate contact with men who have sex with men (and with their contacts). But Ebola is an equal opportunity infection. • AIDS impairs the immune system, so people eventually die of infections that a normal immune system would fight off—but that can often be treated successfully. AIDS does not attack body organs and blood vessels directly. Ebola attacks the immune system first, then many other organs and the blood vessels supplying them, leading to rapid death in up to 90 percent of cases. Past a certain point, the damage is irreversible, even if further viral proliferation could be stopped. • AIDS has never had an explosive outbreak like Ebola’s, which appears to be doubling every three weeks. • AIDS would not be a suitable pathogen for biological warfare; it is not contagious enough, and it does not kill rapidly. Ebola has been viewed as an excellent biological weapon and researched extensively for this purpose. • Both AIDS and Ebola are zoonotic diseases—diseases that long existed in wild animals and “spilled over” into the human population in Africa. AIDS has no known nonhuman reservoir in North America. Ebola appears to be capable of infecting dogs and pigs without sickening the animals. This is why the dog in Spain had to be put down when its owner, a nursing assistant, became infected while caring for a patient.

Reassurances from the CDC, and the public policy based on them, rely on assumptions that are probably not true. The CDC still insists that the virus is not “airborne”—at least not for more than 3 feet. Barack Obama has said that “you cannot get it through casual contact like sitting next to someone on a bus.” But the CDC has told travelers who exhibit Ebola-like symptoms to avoid public transportation.
Our robust and sophisticated medical and public health infrastructure is supposed to be able to handle the situation. Like it did in Dallas? The Dallas public health department is supposed to be carefully following only about 18—how many more does it have the resources to track? It was not following the caregiver who is now infected—she was self-monitoring. The CDC says she must have “breached protocol” though it hasn’t said how. If we have more than 10 or so patients, they can’t be treated in the biosafety-level 4 (BSL-4) facilities that the World Health Organization recommends for this pathogen. They’ll be in places like Texas Health Presbyterian Dallas.

Dr. Jane Orient About the author:Jane M. Orient obtained her undergraduate degrees in chemistry and mathematics from the University of Arizona in Tucson, and her M.D. from Columbia University College of Physicians and Surgeons in 1974. She completed an internal medicine residency at Parkland Memorial Hospital and University of Arizona Affiliated Hospitals and then became an Instructor at the University of Arizona College of Medicine and a staff physician at the Tucson Veterans Administration Hospital. She has been in solo private practice since 1981 and has served as Executive Director of the Association of American Physicians and Surgeons (AAPS) since 1989. She is currently president of Doctors for Disaster Preparedness. Since 1988, she has been chairman of the Public Health Committee of the Pima County (Arizona) Medical Society. She is the author of YOUR Doctor Is Not In: Healthy Skepticism about National Healthcare; Sutton's Law (a novel about where the money is in medicine today); and the second through fourth editions of Sapira's Art and Science of Bedside Diagnosis, published by Lippincott, Williams & Wilkins. She authored books for schoolchildren, Professor Klugimkopf’s Old-Fashioned English Grammar and Professor Klugimkopf’s Spellling Method, published by Robinson Books, and coauthored two novels published as Kindle books, Neomorts and Moonshine, More than 100 of her papers have been published in the scientific and popular literature on a variety of subjects including risk assessment, natural and technological hazards and nonhazards, and medical economics and ethics. She is the editor of AAPS News, the Doctors for Disaster Preparedness Newsletter, and Civil Defense Perspectives, and is the managing editor of the Journal of American Physicians and Surgeons.



